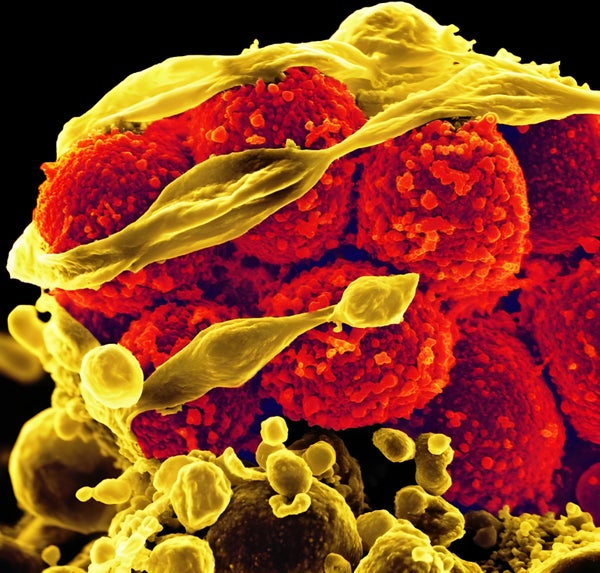
Our skin is crawling with Staphylococcus aureus, the bacterium responsible for most staph infections. Usually staph is harmless, but sometimes—if it breaks through the barrier of our skin or hitches a ride on our food—it can cause severe rashes, food poisoning and even death. For more than a century researchers and clinicians have attempted to find a way to vaccinate against staph infections to no avail. Now researchers point to one possible explanation: staph knows us all too well.
“Staph has developed some type of trick that allows [it] to be able to coexist with humans,” says George Liu, a pediatrician and infectious disease researcher at Rady Children’s Hospital–San Diego. He found it curious that vaccines targeting staph were very successful in animal models but all utterly flopped in human trials, and he began to wonder if there was something about the bacterial host—us humans, that is—that might be preventing development of a successful vaccine.
That is an intriguing idea. But exploring this hypothesis in human experiments turns out to be a tough proposition because many of us are too contaminated to make good test subjects. “One out of three of us are colonized with staph,” Liu says, and nearly 50 percent of human babies are colonized in the first two months of life.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Nevertheless, Liu and his team took it upon themselves to find out why a vaccine against staph failed miserably in humans despite its success in animals. One vaccine other researchers used in clinical trials produced antibodies against IsdB, a protein that is involved in iron uptake. The anti-IsdB vaccine underwent one of the largest phase III trials for staph in 2013, with more than 8,000 participants. Unfortunately, the vaccine was not only ineffective; it also proved more deadly to those who caught staph after they were vaccinated. Liu wanted to know why.
Injecting one set of mice with a salt solution while injecting another group with live staph in the weeks before vaccination allowed the researchers to compare different levels of vaccine efficacy in the two groups. When the disease-free mice were vaccinated, “it was hugely successful,” Liu says. But in mice that had previously had staph, “the vaccine didn’t work at all,” he says. “In fact, what was so surprising was [the efficacy] was a flatline. It did not work. It was 0 percent.”
In this case, Liu found the immune response from a past staph infection rendered any future immune response—even one induced by a vaccine—to be ineffective. When the immune system responded to a natural staph infection instead of a vaccine, the antibodies that targeted IsdB did not actually prevent staph from growing and spreading. These were the antibodies the immune system remembered, so it might be incorrectly presumed that they would guard against illness. In comparison, the antibodies that the disease-free mice generated through vaccination worked just fine to prevent staph. The differing responses do not fully explain why the vaccine’s failure in rodents that experienced a previous infection: if the vaccine was generating protective antibodies in healthy mice, it should still have provided some level of protection in those animals that had previously caught staph.
The culprit seems to be the immune system’s memory of the nonprotective antibodies, which counteracts any positive effect of the vaccine antibodies. This gives staph a two-pronged way of evading the immune system. “[The first] is bringing back the bad antibody, which prevents a lot of good antibodies from forming,” Liu says, “And the second step is: you could have bad antibodies further crowd out and actually outcompete the good antibodies, so they don’t work.” In fact, when previously vaccine-protected mice were dosed with a mixture of human staph antibodies, they lost the protection afforded to them by the vaccine, presumably because the nonprotective antibodies produced by a real staph infection outcompeted those produced from vaccination. When Liu and his team understood why this vaccine failed, they were able to make it work by adding components that changed which section of the IsdB protein was targeted by vaccine-produced antibodies. The results were reported in Cell Host & Microbe.
“Indeed, it is helpful to learn from failures,” such as why the original IsdB vaccine might have failed, says Jan Poolman, head of bacterial vaccines discovery and early development at Janssen Vaccines & Prevention in the Netherlands. Staph vaccines are needed as a public health tool, particularly for older people. Poolman, who was not involved in Liu’s study, thinks that despite the obstacles, this research is a step toward understanding how those vaccines should be developed. “It fits into the growing understanding that a more classical approach to develop a vaccine is not going to be so optimal for Staphylococcus aureus,” he says.
Vaccines are generally developed to target important surface proteins, such as IsdB, under the assumption that the antibodies the immune system produces will incapacitate the virus or bacteria. Liu says that this can work well for diseases that are more novel to humans, such as COVID. When the disease has had the opportunity to figure out how to evade our immune system, however, this classic approach to virology doesn’t work nearly as well. “There’s a list of vaccines that all of us have been struggling to make forever,” he says. “The same principle we’re talking about [with this vaccine] might apply to these hard-to-make vaccines.” Liu plans to further verify that this is an evasion tactic that other strains of staph use and to investigate how the bacterium is actually tricking our immune system. In the meantime, he suggests that understanding that the human immune system may behave differently toward common diseases can be a valuable addition to vaccine development.
More work is needed to develop a fully functional staph vaccine, and researchers will continue to work toward disarming its bag of tricks, Poolman says. His team is working on developing a vaccine that, unlike traditional vaccines, does not attack surface proteins on staph. Instead it targets a toxin staph produces during an infection. “We see a growing number of infectious diseases in adults, particularly older adults, with bacteria like S. aureus,” Poolman says, “That’s why we in vaccinology really are determined to develop this vaccine.”